Suncor Energy Inc. has teamed up with Western University scientists to tackle the shortage of COVID-19 tests, using technology intended to treat wastewater from refineries to produce home testing kits.
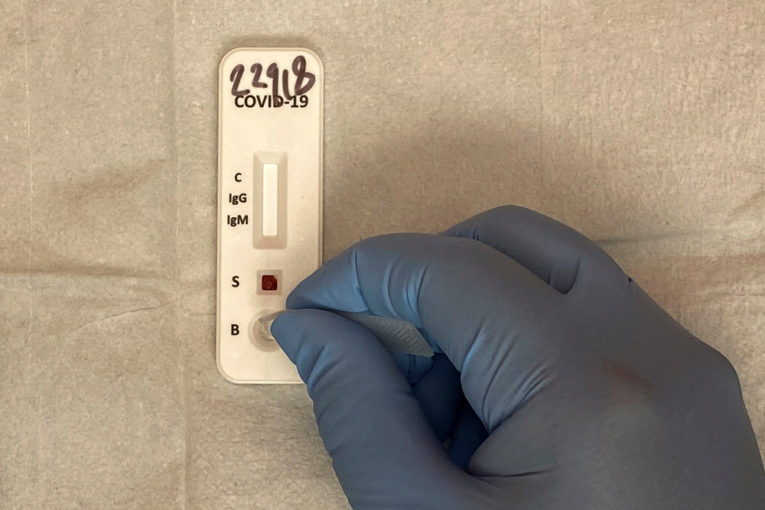
The devices, which could be ready in a few months, would allow individuals to test small samples of bodily fluid, such as blood, for COVID-19 antibodies, and receive the results in minutes.
“We started in mid-March and it’s been going very well,” said Martin Flatley, a senior staff engineer at Suncor’s Sarnia, Ont., refinery. “Western is about 100 kilometres down the road so it’s very easy to visit and bring samples. We’re in constant contact all the time.”
Suncor, the Calgary-based oilsands giant, had already been collaborating with a lab led by Western biochemistry professor Dr. Gregory Gloor when the fast-moving coronavirus swept through North America, forcing closures of non-essential operations and universities.
The team was attempting to identify and sequence genomes of organisms that naturally break down napthenic acid, a toxic byproduct that is part of the wastewater produced by the refinery.
One floor below Gloor’s lab at Western, fellow biochemistry professors David Edgell and Bogumil Karas were working with students to examine a specific type of algae that had been shown to produce proteins in large quantities.
“Their lab is basically next door and we see them all the time, we talk to them all the time, we go out for beers,” said Sam Slattery, a PhD candidate in Edgell’s lab and a lead researcher on the COVID-19 test project.
After the Suncor project was put on hold as COVID-19 hit, the leaders of the two labs wondered if the algae — known as PT algae — could produce the protein necessary to react with COVID-19 antibodies in a test. As part of the process, the Suncor technology could be used to sequence the protein and the algae.
“Someone said ‘let’s see what the algae could do in this situation,’” said Slattery. “Suncor said ‘we’re on board’ and that was it.”
The past couple of months have seen Flatley, Slattery and PhD student David Giguere working around strict university COVID-19 protocols — including a restriction that calls for only one person in the lab at any one time — to produce and sequence the algae and its protein.
The process would be an alternative to current methods, which generate the protein using mammalian and insect cells. That procedure relies on far more costly materials, including a “media” — the rich broth used to grow the protein — that costs about $3,000 a litre compared to pennies a litre for the media used in the algae process.
“The algae is photosynthetic too, so the energy it needs is free, we don’t have to feed it,” said Slattery.
The collaboration, funded by Suncor and Mitacs, a non-profit organization funded by provincial governments to promote innovation, and should have a workable test within a few months.
Epidemiologists have urged countries to dramatically ramp up testing for COVID-19, arguing that identifying and isolating infected individuals is essential to keeping the virus’s spread under control until a vaccine is developed.
The call for testing has become even more urgent as provinces ponder reopening their economies, raising the risk of a second wave of infections. However, fierce global demand for tests has left countries competing for limited supplies as they attempt to develop and ramp up domestic production.

At the moment, the most commonly administered test is the nasopharyngeal swab, which identifies the active presence of the virus. The 6-inch swab is inserted through the nose by a medical professional.
However, scientists have been anxiously awaiting the development of both at-home tests and antibody tests that could measure those that have already been infected. Enabling individuals to administer their own tests could dramatically improve existing data on infections, particularly since the disease is carried by asymptomatic individuals.
“If you have antibodies, you are probably over the infection,” said Barry Bloom, a professor of public health at Harvard University and a specialist in infectious diseases. If you don’t have the antibodies and don’t have symptoms, that’s where you’re at risk of being infected, you’re a threat. But the only way to know that is to test.”
Financial Post
• Email: [email protected] | Twitter: naomi_powell
You can read more of the news on source
